Antibiotics have saved millions of lives. They treat bacterial infections such as pneumonia, urinary tract infections, and wound infections. But these powerful medicines are losing their effectiveness.
Antibiotic resistance is one of the biggest health threats in the world today. It makes common infections harder to treat and increases the risk of serious illness and death.
Understanding why antibiotic resistance is dangerous can help protect you, your family, and the community.
What Is Antibiotic Resistance
Antibiotic resistance happens when bacteria change in a way that makes antibiotics no longer work against them.
This does not mean your body becomes resistant. It means the bacteria become stronger and survive the medicine designed to kill them.
As a result, infections last longer and become harder to treat.
Why Is Antibiotic Resistance Dangerous
Antibiotic resistance is dangerous for several serious reasons.
1. Common Infections Become Harder to Treat
Infections that were once easy to cure can become severe. Doctors may need to use stronger, more expensive medicines with more side effects.
In some cases, no effective antibiotic is available.
2. Higher Risk of Complications and Death
When infections cannot be treated properly, they may spread to the blood or vital organs.
This increases the risk of hospitalization and death.
3. Longer Hospital Stays
Patients with resistant infections often require longer treatment and isolation in hospitals. This increases healthcare costs and emotional stress.
4. Routine Medical Procedures Become Riskier
Modern medicine depends on antibiotics.
Procedures such as:
• Surgery
• Chemotherapy
• Organ transplants
• Childbirth
• Treatment of premature babies
All rely on antibiotics to prevent or treat infections. Without effective antibiotics, these procedures become much more dangerous.
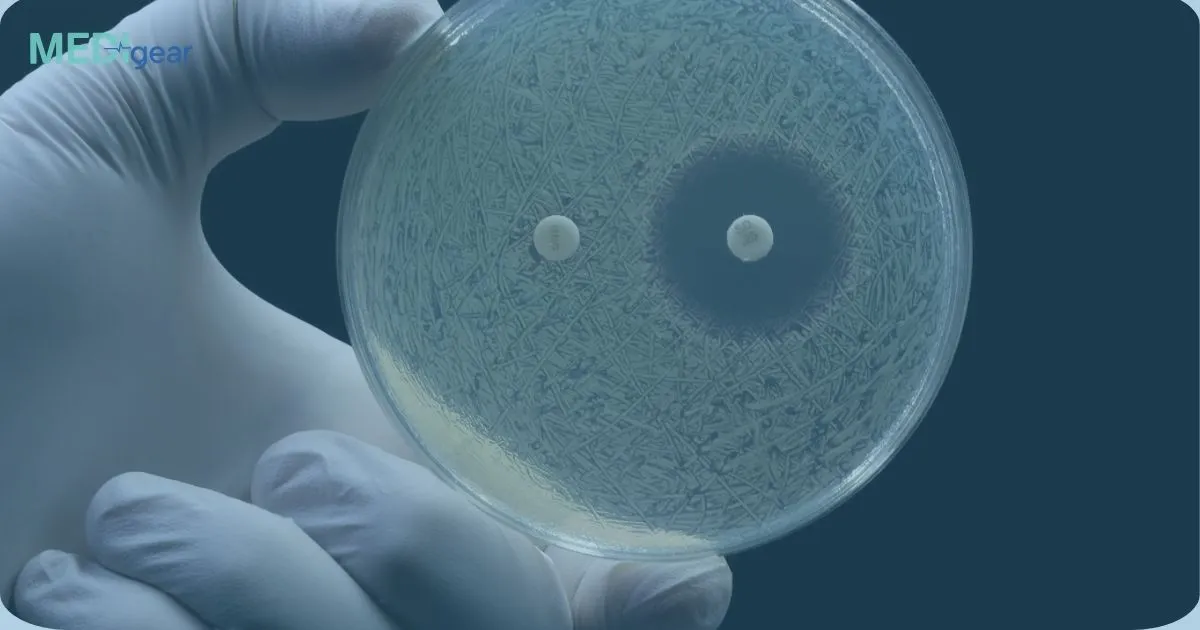
5. Spread of Superbugs
Some bacteria develop resistance to multiple antibiotics. These are sometimes called superbugs.
These resistant bacteria can spread between people, in hospitals, and even through food and the environment.
How Does Antibiotic Resistance Happen
Antibiotic resistance develops naturally over time, but misuse speeds it up.
Common causes include:
• Taking antibiotics for viral infections like colds or flu
• Not completing the full course of antibiotics
• Overuse of antibiotics in humans
• Use of antibiotics in livestock and agriculture
• Poor infection control in hospitals
The more antibiotics are used incorrectly, the faster bacteria adapt and become resistant.
Examples of Resistant Infections
Resistant infections can affect many parts of the body, including:
• Tuberculosis
• Urinary tract infections
• Skin infections
• Pneumonia
• Bloodstream infections
Some resistant infections require hospital treatment and intravenous antibiotics.
Why This Is a Global Problem
Antibiotic resistance does not stay in one country. Resistant bacteria can spread through travel, food trade, and human contact.
This makes antibiotic resistance a global public health emergency.
If action is not taken, minor injuries and common infections could once again become life threatening.
How Can We Prevent Antibiotic Resistance
Everyone has a role to play.
Use Antibiotics Responsibly
• Only take antibiotics when prescribed by a qualified healthcare professional
• Do not demand antibiotics for viral illnesses
• Complete the full course as prescribed
• Never share antibiotics with others
Practice Good Hygiene
• Wash hands regularly
• Keep wounds clean
• Stay up to date with vaccinations
Vaccines reduce infections and lower the need for antibiotics.
Support Infection Control
Hospitals and clinics must follow strict hygiene practices to prevent the spread of resistant bacteria.
The Bottom Line
Antibiotic resistance is dangerous because it makes infections harder to treat, increases the risk of serious illness, and threatens modern medical care.
Responsible antibiotic use, strong hygiene practices, and public awareness are key to slowing this growing threat.
Protecting antibiotics today ensures they remain effective for future generations.