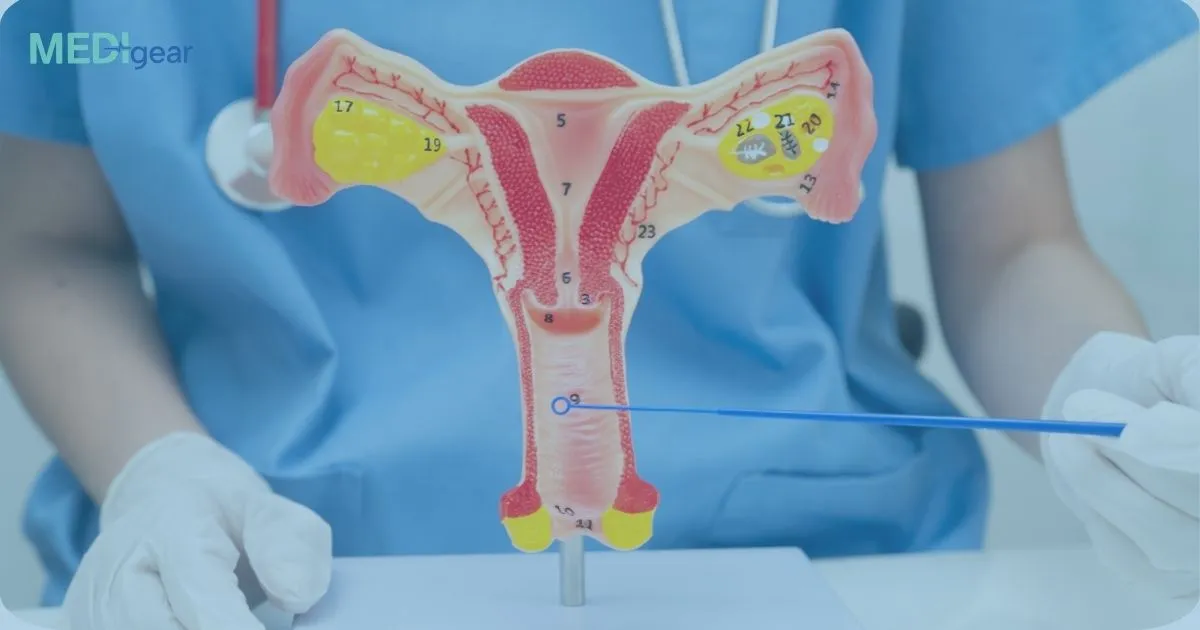
What Is HPV and Why Screening Matters
Human papillomavirus, commonly called HPV, is a very common infection. Most infections clear naturally without causing harm. However, certain high-risk HPV types can lead to cervical cancer if they persist over time.
Cervical cancer is the fourth most common cancer in women worldwide. Regular screening helps detect high-risk HPV infections before they cause serious cell changes.
Health experts generally recommend HPV testing every 5 years for people aged 30 to 65 who have a cervix. The standard method involves collecting cervical cells during a pelvic exam.
While effective, traditional screening methods can feel uncomfortable or embarrassing for some people. This leads to missed appointments and lower screening rates.
What Did the New Study Find
A large study conducted in China and published in The British Medical Journal evaluated whether menstrual blood could detect HPV as accurately as clinician-collected cervical samples.
Study Overview
• Over 3,000 women aged 20 to 54 participated
• Each provided menstrual blood using a mini pad
• Two additional cervical samples were collected by clinicians
• Researchers compared accuracy across methods
Key Results
• Sensitivity of menstrual blood testing: 94.7 percent
• Sensitivity of clinician cervical samples: 92.1 percent
• Specificity of menstrual blood testing: 89.1 percent
• Specificity of cervical samples: 90 percent
• Negative predictive value for both methods: 99.9 percent
This means that menstrual blood testing was almost as accurate as traditional cervical sampling for detecting high-grade precancerous lesions.
A negative result was highly reliable in ruling out serious disease.
How Does Menstrual Blood HPV Testing Work
Instead of undergoing a pelvic exam, individuals collect menstrual blood at home using a mini pad attached to a regular sanitary pad.
The pad is then sent for laboratory testing to detect high-risk HPV strains.
This method removes the need for a speculum exam and clinician involvement during sample collection.
Why This Could Be a Game Changer
1. Less Invasive- No pelvic examination is required. For people who experience discomfort, trauma, or cultural barriers, this is a major advantage.
2. More Privacy- Testing can be done at home during normal menstruation.
3. Increased Accessibility- This option may help people in rural or underserved areas who struggle to attend clinic appointments.
4. Potential to Improve Screening Uptake- People who avoid screening due to embarrassment or fear may be more willing to participate with a home-based method.
Who May Benefit Most
Menstrual blood testing could be especially helpful for:
• People who avoid pelvic exams
• Those with past traumatic experiences
• Individuals living in remote areas
• People who prefer at-home health testing
However, this method may not work for everyone.
It is only suitable for individuals who menstruate regularly. It may not be appropriate for:
• Postmenopausal individuals
• People on hormonal treatments that stop periods
• Those with very irregular menstrual cycles
Are There Any Limitations
Although the results are promising, the study was observational. More research is needed in different countries and populations to confirm effectiveness in real-world screening programs.
Experts also note that patient experience data is still missing. It is important to understand how easy and convenient people find this method.
Before being added to national screening guidelines, further validation will be required.
Could This Replace Pap Smears
At this stage, menstrual blood HPV testing is not replacing standard screening. However, it may become an additional option in the future.
It could serve as:
• An alternative self-sampling method
• A tool to reach people who skip regular screening
• A complementary approach in screening programs
If validated in larger studies, it could expand access to life-saving cervical cancer prevention.
The Bottom Line
Menstrual blood HPV testing is a promising innovation in cervical cancer screening. It offers a noninvasive, convenient, and potentially more accessible option for detecting high-risk HPV infections.
If future studies confirm its effectiveness across diverse populations, it could help improve screening participation and reduce cervical cancer rates worldwide.
Early detection saves lives. Expanding screening options may be one of the most important steps toward better prevention.